Self-sampling by women for cervical cancer screening promises to be highly effective clinically, though practical hurdles remain in terms of implementation on a large scale, according to new studies reported this week.
In a large U.S. study conducted by Kaiser Permanente Washington, women who were overdue for cervical cancer screening were sent home-testing kits for HPV, but only about 12% sent them back. And though the screening rate was improved, the rate of detection for precancerous lesions was not significantly higher. In addition, a sizeable percentage of those with the most worrisome findings failed to follow up with colposcopy as they should have, according to results published November 6 in JAMA Network Open. Nevertheless, researchers have cause for optimism.
"This study indicates that mailing [HPV] kits to underscreened women can increase cervical cancer screening, and implementation efforts should strategize how to further increase kit uptake and follow-up of positive results to maximize detection and treatment of precancers in women at high risk," wrote lead author Rachel Winer, PhD, a professor of epidemiology at the University of Washington School of Public Health, and colleagues.
Separately, researchers at Queen Mary University of London reported a good experience with their investigational "S5" DNA methylation panel as used in vaginal and urine samples taken by women at home. They shared their results in a poster presentation on November 4 at the U.K. National Cancer Research Institute (NCRI) meeting in Glasgow.
Missing out on cervical cancer screening
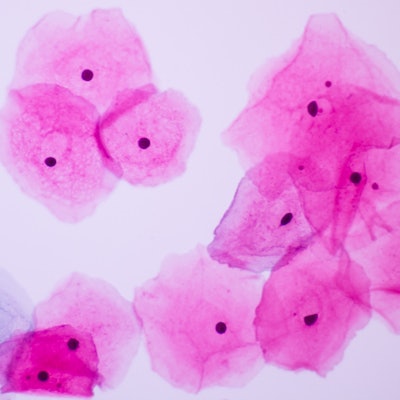
Home testing represents a potential solution for the problem of underscreening for cervical cancer -- that is, for women who do not have access to Pap and HPV tests that can pick up on cancer risk and signs of dysplasia early enough for an intervention. More than half of women diagnosed with cervical cancer in the U.S. were underscreened, Winer and colleagues noted.
"Well-documented barriers include lack of time or transportation, difficulties finding childcare or taking time off work, fear of pelvic examinations, and prior negative experiences with screening," they wrote.
In contrast with traditional Pap tests, which need to be sampled by a professional, HPV tests can be reliably done on samples taken by women themselves at home. In theory, this could boost compliance, though more U.S. data are needed to show how this would work in practice in health systems, the authors wrote.
The Kaiser study -- dubbed Home-Based Options to Make Cervical Cancer Screening Easy (HOME) -- was designed to see if mailing home-testing kits to enrollees who had not had a Pap test within three years and five months would help identify cases of cervical intraepithelial neoplasia (CIN) grade 2 or higher. Women in need of screening were identified through electronic medical records. The researchers compared outcomes for standard reminders versus standard reminders plus a mailed HPV self-testing kit in a total of 19,581 Kaiser enrollees.
In the group that received the test kits, 26.6% went on to get follow-up screening, compared with 17% of those who only received the usual patient reminders; the difference was statistically significant, the researchers noted. However, there was no statistically significant difference in the number of precancers detected or treated. In a worrying finding, among those who had abnormal results, 67.1% in the intervention group and 83.3% in the control group went on to get a colposcopy as needed, so many still did not get the correct follow-up care.
A low rate of return
The researchers also pointed out that among 9,960 women who received the home kits, only 12.1% returned them and 14.5% headed to the clinic for screening instead.
Dr. Jenell Coleman Fennell, director of gynecologic specialties at Johns Hopkins, and colleagues expressed disappointment in the low rate of return in an accompanying editorial in JAMA Network Open.
"While the trial is admirable in its design and large sample size, several limitations prevent it from having broad implications for cervical cancer screening at this time," they wrote.
The low rate of return may have been due to instructions to undergo clinic-based screening regardless of home HPV screening, Coleman Fennell and colleagues speculated. Or it may have been due to uncertainty among participants about the value of the home kits because vaginal HPV testing is not approved in the U.S. for risk stratification in cervical cancer screening. The editorial writers also found the increase in the screening rate for the home kit group over usual care to be "modest" and noted the low prevalence of dysplasia in the population.
What's more, the population in the study is healthier and more stable than would be expected. Underscreened women may not have health insurance or a stable address where a kit can be mailed. However, on the positive side, the study shows that it's possible for large health systems to implement a home HPV screening program, they concluded.
DNA methylation test shows promise
Meanwhile, researchers in the U.K. have been experimenting with at-home sampling for women, with results tested using a DNA methylation panel in urine and vaginal samples. The DNA methylation panel -- called the S5 classifier -- was developed at Queen Mary University of London. It tests for four high-risk HPV types (HPV16, HPV18, HPV31, and HPV33) and EPB41L3, which is understood to be a tumor suppressor gene. A risk score is assigned based on the results, with higher scores suggesting greater risk for cancer (Lorincz et al, International Journal of Cancer, June 1, 2016, Vol. 138:11, pp. 2745-2751).
The researchers tested the classifier in a study of 600 women attending the colposcopy clinic at the Royal London Hospital to follow up on an abnormal Pap test with or without an abnormal HPV test result. The findings were detailed in a poster presentation at the NCRI meeting by Dr. Belinda Nedjai, a senior research fellow and director of the molecular epidemiology lab at Queen Mary University, and colleagues.
All 600 study participants submitted two vaginal samples, and 503 also provided a urine sample. All samples were tested with the S5 classifier and for high-risk HPV (hrHPV) using the Becton Dickinson Onclarity test.
A higher S5 score was associated with more severe disease in all samples tested, the researchers reported. Furthermore, they concluded that the S5 classifier had similar sensitivity as the high-risk HPV assay, but with better specificity on all devices tested (see table). The Dacron wet swab and Qvintip dry swab produced the best results.
The researchers said in a statement that women "much preferred" home testing to testing at a doctor's office, though supportive data were not reported in the poster presentation. Home testing appears to be a good option for women who do not participate in cervical cancer screening programs or who do not follow up on abnormal results, and it has much potential for even broader use, they concluded.
| Comparison of S5 classifier vs. hrHPV* test | |||
| Home sampling | Test type | Sensitivity | Specificity |
| Urine testing | |||
| Colli-Pee (Novosanis) | hrHPV | 82.3% | 29.3% |
| S5 | 83.3% | 45.5% | |
| Vaginal swab testing | |||
| Wet swab (Dacron) | hrHPV | 88.2% | 32.2% |
| S5 | 88.2% | 36.7% | |
| FloqSwab dry (Copan Diagnostics) | hrHPV | 85.3% | 32.2% |
| S5 | 85.3% | 41.3% | |
| HerSwab dry (Eve Medical) | hrHPV | 61.3% | 39.5% |
| S5 | 62.5% | 53% | |
| Qvintip dry (Approvix) | hrHPV | 72.7% | 35.7% |
| S5 | 73.5% | 68.6% | |