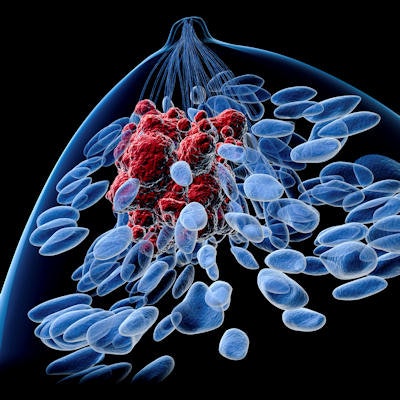
A study published April 30 in Breast Cancer Research and Treatment provides more support for the use of genetic testing to tailor adjuvant treatment for breast cancer patients based on their predicted risk of disease recurrence.
The study focused on 3,746 pre- and postmenopausal women with estrogen receptor (ER)-positive, human epidermal growth factor receptor 2 (HER2)-negative breast cancer who had participated in clinical trials. It was led by Ivana Sestak, PhD, from Queen Mary University of London, and data were previously presented at the San Antonio Breast Cancer Symposium in December 2018.
The researchers found that scores for risk of breast cancer recurrence using the EndoPredict assay (Myriad Genetics) correlated with outcomes, as measured by 10-year distant recurrence-free interval (DRFI) rates, according to the study, which was funded by Cancer Research UK and Myriad Genetics.
The test was "highly prognostic for women with ER-positive, HER2-negative breast cancer who received endocrine therapy alone and in those who received chemotherapy plus endocrine therapy," Sestak et al wrote.
Tests may spare chemo use
Many factors are considered in determining a patient's prognosis and treatment, including a range of pathological and molecular characteristics of the tumor, the researchers noted.
"Almost all women with ER-positive, HER2-negative breast cancer will receive at least 5 years of endocrine therapy but the question who will benefit from adjuvant chemotherapy is more challenging," they wrote.
The EndoPredict test is a 12-gene quantitative polymerase chain reaction (qPCR) assay that incorporates tumor size and nodal status to generate a patient's risk of 10-year recurrence for cancer. The test generates a molecular score that can be combined with tumor size and lymph node status to provide what's called an EPclin risk score on a scale of 1 to 6, with 1 denoting the lowest risk and 6 the highest risk.
EndoPredict has proved its abilities in terms of predicting outcomes, but it has not been clear whether the assay could be used to predict the benefit of chemotherapy, the researchers noted. The current study was designed to help show the role of testing in making this assessment, using a score of 3.3 as a cutoff point delineating low versus high risk.
The breast cancer patients evaluated in the study had all received endocrine therapy alone or with chemotherapy for five years.
Data were drawn from five large trials:
- Spanish Breast Cancer Group (GEICAM) 9906 (n = 500)
- GEICAM 2003/02 (n = 616)
- Austrian Breast and Colorectal Cancer Study Group (ABCSG) 6 (n = 378)
- ABCSG 8 (n = 1,324)
- Translational substudy of the Arimidex, Tamoxifen, Alone or in Combination trial (TransATAC) (n = 928)
Tissue samples were available for all five trials and were analyzed with EndoPredict at Myriad Genetics by researchers blinded to the outcomes data.
As the primary end point, the study assessed whether the participants had a distant recurrence over 10 years and compared this with their EPclin score. As a secondary end point, the researchers looked at the breast cancer-free interval over 10 years, meaning participants were free of local and distant recurrences.
Results for women in the GEICAM studies, who had been treated with hormone therapy and chemotherapy, were compared with results for those enrolled in the ABCSG and TransATAC trials, who had hormone therapy alone.
The patients who received endocrine therapy alone had a significantly lower median EPclin score than the women in the other trials (3.07 versus 3.67), the researchers noted.
Interpreting higher risk scores
Among patients with an EPclin score of 5, the 10-year rate of distant disease recurrence was 46% for those who had endocrine therapy alone, compared with 26% for those who received hormonal therapy plus chemotherapy. The different was statistically significant.
"Overall, our analysis suggests that women with high EPclin scores [benefited] from chemotherapy compared to those with the same EPclin score but receiving endocrine therapy alone, irrespective of node-positivity of the disease," Sestak and colleagues wrote.
Conversely, there were no differences in the rate of distant recurrence at 10 years for those with low EPclin scores, regardless of whether the women had endocrine therapy alone or endocrine therapy with chemotherapy. This suggests some women with low EPclin scores were overtreated with chemotherapy, the researchers concluded.
As for the secondary end point of breast cancer-free survival, results were similar. For those with an EPclin score of 5, the risk of 10-year recurrence was 57% for endocrine therapy alone versus 29% for endocrine therapy with chemotherapy. EPclin was highly prognostic for women treated with endocrine therapy and for those who received endocrine therapy and chemotherapy, according to the researchers.
Results in line with other trials
Sestak and colleagues acknowledged that the retrospective design was a limitation of the study, but they also noted that the results are "consistent with other studies that demonstrate chemotherapy benefit for patients with high-risk disease based upon molecular analyses."
In addition to EPclin, a range of other genetic test risk scores are available, including the Oncotype DX breast recurrence score (Genomic Health) and the Breast Cancer Index (Biotheranostics).
In the Trial Assigning Individualized Options for Treatment, or TAILORx, women with hormone receptor-positive, HER2-negative breast cancer and no lymph node involvement who had a midrange score on the Oncotype DX test had similar outcomes with endocrine therapy alone and endocrine therapy with chemotherapy. The prospective study was sponsored by the U.S. National Cancer Institute and reported in mid-2018.
"The current analysis approach can facilitate insight into the predictive value of EPclin for women with ER-positive, HER2-negative breast cancer," Sestak and colleagues concluded.