The Society of Critical Care Medicine (SCCM) unveiled a new program to cut deaths from sepsis in low- and middle-income countries (LMICs) with ambitions to improve access to diagnostic tools, laboratories, and medicines at its 2024 Critical Care Congress held in Phoenix from January 21 to January 24.
The seven-year program, entitled “Reducing Mortality from Sepsis in Low-Resource Settings,” has received $705,000 in funding from the Laerdal Foundation for the first two of its four phases.
Sepsis, a life-threatening response to an existing infection, kills about 11 million of the 50 million people worldwide who are affected by it. About 85% of sepsis cases and 84% of sepsis deaths occur in LMICs with scarcer resources such as antibiotics and equipment.
“Early identification and effective treatment are vital to effectively managing sepsis,” said Dr. Jorge Hidalgo, president of the World Federation of Intensive and Critical Care and head of the intensive care unit at Belize Healthcare Partners.
“That is a challenge in low-resource settings due to the limited training, access to healthcare resources, infrastructure, therapies, and tools. The initiative aims to address these significant gaps and access to essential resources, which requires a multifaceted, multiprofessional approach,” said Hidalgo, who will help lead the program’s initial phases.
The SCCM said that filling critical gaps will require action across many fronts, such as improving early recognition and diagnosis and access to antibiotics, better infection control at healthcare facilities to avert sepsis outbreaks, more effective emergency and critical care, training of staff to monitor patients’ responses to therapies, and patient education.
The organization noted that low-resource settings suffer from a lack of robust data on sepsis incidence, interventions, care processes, and outcomes. They also face shortages of key staff including physicians, nurses, respiratory therapists, and laboratory technicians, along with shortages of essential medicines, ventilators, and other equipment.
The program is being launched under the Surviving Sepsis Campaign (SSC), which was established in 2002 by SCCM and the European Society of Intensive Care Medicine (ESICM).
Phase 1 will involve surveying clinicians to assess needs, summarize the evidence base, and identify gaps in knowledge; phase 2 will entail creating toolkits and resources, and capturing how these are used.
The first two phases will be led by Hidalgo and Samuel Akech, PhD, director of CDC Western Kenya for the U.S. Centers for Disease Control and Prevention (CDC) in Kenya.
With phase 2 due for completion in September 2025, SCCM is pursuing funding for phases 3 and 4, which will focus on implementing, disseminating, and assessing impact in 20 global regions.
“SCCM is launching this project through the SSC, whose guidelines have been shown to reduce deaths from sepsis in adults and children and improve overall outcomes, but are better aligned to places with more resources, such as the United States and Europe,” said Dr. Vinay Nadkarni, immediate past president of SCCM.
“Ultimately, the SSC guidelines will be expanded and updated to reflect the findings and recommendations discovered by this initiative,” Nadkarni said.
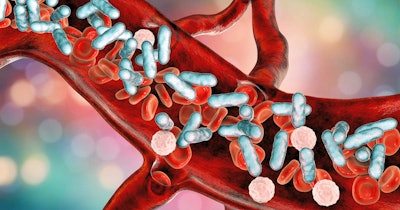
In another presentation at the SCCM Critical Care Congress, data was presented comparing the performance of the SeptiCyte RAPID (SeptiScore) test at differentiating sepsis from systemic inflammatory response syndrome (SIRS) relative to other diagnostic tests commonly used to identify sepsis.
The data was taken from 10 hospital sites in the U.S. and Europe with a patient cohort that included critically ill adults admitted to intensive care with a suspicion of sepsis.
The test, which measures two immune biomarkers to differentiate sepsis from SIRS, is produced by Immunexpress, a molecular diagnostic company based in Brisbane, Australia and Seattle.
The test uses reverse transcription polymerase chain reaction (RT-PCR) to quantify the relative expression levels of host response genes isolated from whole blood, providing results in about an hour from sepsis suspicion. It is intended for use in conjunction with clinical assessments, vital signs, and laboratory findings on patients with escalating signs and symptoms of critical illness.
"The data demonstrate that no combination of biomarkers outperformed SeptiScore alone, or models including SeptiScore, at identifying sepsis," said Dr. Roy Davis, PhD, chief medical officer of Immunexpress in the presentation.
Davis said SeptiCyte RAPID was not intended to be used as a standalone test, but in this study “adding other biomarkers to SeptiScore didn't appreciably increase the diagnostic certainty of differentiating sepsis from SIRS.”