Administering a protein that correlates to survival in sepsis has improved survival in mice in a study, pointing to a potential new way to treat the life-threatening reaction to infection.
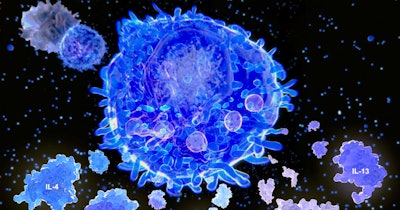
Each year, sepsis affects almost 50 million people, around 11 million of whom die. Patients with sepsis have an excessive, cytokine-mediated host inflammatory response after their immune response fails to contain an infection. Later, an anti-inflammatory response can become immunosuppressive, putting the patient at risk of harm from the initial infection and potential secondary infections.
Treatment options are limited, in part because of a lack of clarity about what drives the unbalanced immune response. Writing in Science Translational Medicine, a team at Chongqing Medical University in China described their work to identify the drivers and discover a potential new treatment option.
The researchers looked at biomarkers in two independent cohorts of patients. In the discovery cohort, which comprised 68 patients with sepsis and 30 healthy volunteers, the researchers found patients with septic shock had significantly lower concentrations of serum bone morphogenetic protein 9 (BMP9). The cytokine has been shown to play a protective role in people with inflammation-induced lung injury.
Serum BMP9 concentrations at admission were significantly lower in sepsis patients than in healthy people in both the discovery cohort and the 434-person validation cohort. Concentrations were also significantly lower in people who died of sepsis than in those who survived.
The biomarker analysis led the scientists to assess the effect of giving a recombinant form of the BMP9 protein to mice. After inducing sepsis in mice and triggering a significant drop in BMP9 concentrations in the process, the researchers injected various doses of the protein or a control.
Between 80% and 100% of the mice died in the absence of treatment. Early treatment with the protein reduced the mortality rate to around 50% at the lowest dose, and lower still at the two higher doses. The BMP9 protein was less effective when given after six or 12 hours, but was still associated with significant improvements in survival.
“BMP9 replacement therapy enhanced bacterial clearance and improved survival in sepsis by activating macrophages in an ALK1 and Smad1/5-dependent manner. Thus, these data lay the foundation for future studies guiding the development of personalized BMP9-based immune therapies for sepsis,” the authors of the paper wrote.



















