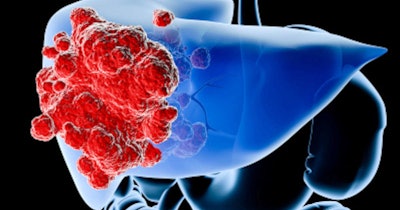
Certain gene mutations could serve as markers to help physicians predict which patients with hepatocellular carcinoma are most likely to develop resistance to the drug lenvatinib. The findings, published in Gastroenterology, could one day help clinicians better identify patients that may benefit from alternative treatments.
According to the Centers for Disease Control and Prevention (CDC), more than 35,000 people in the U.S. are diagnosed with liver cancer annually. Hepatocellular carcinoma is the most common form of primary liver cancer. For about one-fourth of hepatocellular carcinoma patients whose cancers cannot be treated with surgery or liver transplantation, lenvatinib is effective in stopping tumor growth. For others, drug resistance in hepatocellular carcinomas is common but not well understood.
In this retrospective study, researchers analyzed the genetic profiles of circulating tumor DNA shed from cancer cells and disseminated into the bloodstream for 46 patients who underwent hepatocellular carcinoma treatment at the University of Texas (UT) Southwestern Medical Center and Parkland Memorial Hospital. Sixteen patients were treated with lenvatinib, and 30 with immunotherapy drugs. By examining circulating tumor DNA collected both before treatment and after cancers had progressed with treatment, the research team could identify differences in the genetic profiles of cancers once they were resistant to treatment.
In patients who received lenvatinib, the number of mutations in the genes EGFR and ERBB2, as well as the number of copies of the genes present in cancer cells, tended to increase. Those changes were not seen in patients treated with other drugs, suggesting that the change was a response to lenvatinib. EGFR and ERBB2 were previously known to play a role in cell growth and are mutated in many cancer types.
The team carried out an additional analysis of 227 patients treated for hepatocellular carcinoma at cancer centers nationwide. About 62.5% of patients without EGFR or ERBB2 mutations before treatment showed tumor shrinkage or stability after starting lenvatinib compared with 20% of those who had EGFR or ERBB2 mutations. On average, patients whose tumors had EGFR or ERBB2 mutations had lower survival rates than those whose tumors lacked the mutations.
Using a national cohort of 1,616 patients, researchers calculated that about 11% of hepatocellular carcinoma patients have EGFR or ERBB2 mutations. Since these patients are less likely to respond to lenvatinib, they could potentially be offered alternative or combination treatments. Unlike most hospitals, UT Southwestern Medical Center now routinely analyzes for genetic mutations present in hepatocellular carcinomas.
“These findings can potentially guide future clinical trials on how to prevent and treat lenvatinib resistance in hepatocellular carcinoma as well as other cancers,” lead author Dr. David Hsieh, assistant professor of internal medicine at UT Southwestern Medical Center, said in a statement. “This research may define a new marker to select patients for specific treatments. It also suggests that drugs targeting EGFR and ERBB2 combined with lenvatinib may be a very effective treatment in select patients.”