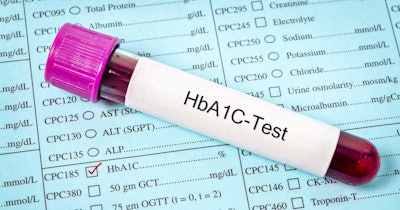
Type 2 diabetes is often asymptomatic and frequently remains undiagnosed, unless caught in routine screening or if symptoms develop. Given the health risks of type 2 diabetes and the social costs and impact of the disease, especially when undiagnosed and unchecked, many countries have implemented HbA1c screening programs to diagnose and treat diabetes as early as possible in at-risk individuals.
However, there has been little data analysis to quantify the effectiveness of HbA1c screening programs in catching type 2 diabetes in undiagnosed patients. How much earlier do these programs identify undiagnosed cases of type 2 diabetes than occurs in the course of routine care?
A new study published in Diabetologia from the U.K., led by Drs. Katie Young, John Dennis, and Nicholas Thomas at the University of Exeter, used clinical data from the UK Biobank to approach this question.
Among the main findings, they noted that HbA1c screening in adults between 40 and 70 years of age can reduce the time to diabetes diagnosis by a median of 2.2 years compared with routine clinical care.
The study used data from 179,923 individuals 40 to 70 years of age; 13,077 had been diagnosed with type 2 diabetes previously. The researchers established an elevated HbA1c level of ≥48 mmol/mol (≥6.5%) to identify those with undiagnosed diabetes among the remaining 166,846 members of the cohort.
Using this HbA1c level as the baseline for diabetes, the data showed that 1,703 (1%) of individuals without a diabetes diagnosis did in fact have undiagnosed diabetes, representing an additional 13% of diabetes cases in the study population. Furthermore, the median time to diagnosis (calculated as the time elapsed between enrollment in the UK Biobank and diagnosis) for those with undiagnosed diabetes was 2.2 years. Within 10 years of follow-up, 88% of the individuals with undiagnosed diabetes had received a clinical diagnosis.
With approximately 25 million adults without a diabetes diagnosis in the age range of 40 to 70 years in the U.K., the 1% of undiagnosed cases found in the data could mean that there are 250,000 undiagnosed (and untreated) cases of type 2 diabetes in the country in that age group.
The study authors point out that the data in the UK Biobank are not representative of the larger U.K. population in significant ways; they note that these limitations in the data inherently limit their study. First, the data in the UK Biobank generally come from healthier (and more health-conscious) individuals who are generally from higher socioeconomic strata; moreover, data from individuals from minority groups, including those who are Black or South Asian -- who are at higher statistical risk of developing adult-onset diabetes -- is lacking in the UK Biobank.
These two points suggest that the percentage of undiagnosed cases in the 40 to 70 age range in the U.K. may be significantly higher than 1%. In fact, the Diabetes UK organization estimates that there may be 850,000 people in the U.K. living with undiagnosed type 2 diabetes.
The findings also show that in the group of 1,703 people with undiagnosed diabetes, the longest delays before diagnosis were for women and those with a lower BMI (and women with lower BMIs in particular), as well as those with lower -- but still indicative of diabetes -- HbA1c levels. The authors note that this may indicate that clinicians are less likely to consider women and people with BMIs under the obese range as being at risk for diabetes.
With these considerations, the authors note that “selective screening strategies based on validated risk scores can reduce the number needing to be screened by approximately half” but point out that solely employing these strategies may miss 15% to 30% of undiagnosed cases of diabetes, especially in ethnic-minority populations, women, and those with lower BMI scores.
The study acknowledges the challenge presented to broader screening initiatives in the U.K. by the decrease in healthcare spending due to the widespread economic downturn. However, the authors point out that diabetes screening initiatives might be more important than ever in the current climate, as earlier diagnosis allows earlier intervention, reducing the risk of diabetes complications. Furthermore, the authors note that HbA1c screening is currently the most reliable method for identifying undiagnosed diabetes.
While the authors note in their conclusion that their study is the first population-based analysis of the effect of an HbA1c screening program on the time to diagnosis of type 2 diabetes, they stress that more evaluation should be done to provide a better and more comprehensive picture: “Earlier diagnosis would allow earlier intervention with the potential to reduce the risk of diabetes complications, but this requires further evaluation.”