Strata Oncology, a precision oncology company, has announced the publication of a peer-reviewed study validating the clinical utility of its solid tumor predictive biomarker for checkpoint inhibitor immunotherapy benefit.
The study, published on Tuesday in Communications Medicine, presents opportunities to expand immunotherapy benefits to more patients.
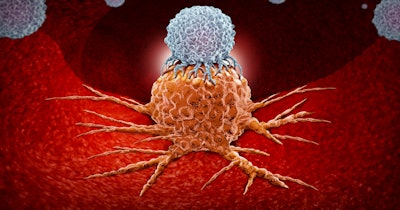
Checkpoint inhibitors, therapies that regulate the immune system, have greatly improved the treatment of patients with advanced cancer. The checkpoint inhibitors anti-PD-1 and anti-PD-L1 monoclonal antibodies are approved for use in multiple tumor types. Current pan-tumor biomarkers (relevant to many types of tumors) for these treatments identify only a fraction of responsive patients. Therefore, many people who could benefit from these therapies are not being identified. Additionally, immunotherapy is now often combined with chemotherapy.
New data in non-small cell lung cancer indicates that Strata’s Immunotherapy Response Score (IRS), the biomarker for anti-PD-1/PD-L1 checkpoint inhibitor monotherapy benefit, may be a useful tool to help determine which patients can achieve these benefits without chemotherapy’s toxic effects.
The precision oncology company combines molecular profiling, real-world data, and a large-scale clinical trial platform to identify and deliver optimal treatments for patients with cancer.
Using treatment data and clinical molecular test results, researchers conducting the Communications Medicine study reported the development and validation of IRS to predict checkpoint-inhibitor benefit. Across patients with more than 20 advanced cancer types, IRS predicted checkpoint-inhibitor benefit better than currently available tests. Data from more than 20,000 patients showed that IRS identifies about 8% of patients with advanced cancer who may benefit significantly from checkpoint inhibitors but would not receive them today based on currently available tests.
The researchers found that IRS predicted real-world progression-free survival and overall survival in anti-PD-1/PD-L1 monotherapy-treated patients across tumor types. IRS-high status predicted similar duration of benefit across tumor types as did another measure, tumor mutational burden-high status, but identified twice as many patients who could benefit from checkpoint-inhibitor treatment. In non-small cell lung cancer patients who were IRS-high, there was no significant benefit of combination therapy (pembrolizumab + chemotherapy) compared to monotherapy (pembrolizumab).
Researchers say the Immunotherapy Response Score meets a need for an integrative diagnostic test that better predicts the likelihood of benefit from anti-PD-1/PD-L1 checkpoint inhibitor monotherapy across solid tumor types. This approach may help clinicians decide which patients should receive checkpoint inhibitors to treat their disease.
“Immunotherapy has transformed cancer care and now with IRS we have the ability to predict benefit across tumor types,” said Strata Oncology co-founder and CEO Dan Rhodes, in a statement.