Researchers have revealed how immune cells are spatially organized within some tumors and that certain immune “hubs” may be linked to better cancer treatment responses.
The study, detailed in Nature Immunology, sheds light on the organization of immune cells in human tumors, which has not been well understood.
Scientists have been trying to figure out why most patients with cancer who are treated with immunotherapies called PD-1 inhibitors don’t respond to the treatments. A team at the Broad Institute of Massachusetts Institute of Technology (MIT) and Harvard, Brigham and Womens’ Hospital and Massachusetts General Hospital (MGH) focused on non-small cell lung cancer (NSCLC), the leading cause of cancer deaths.
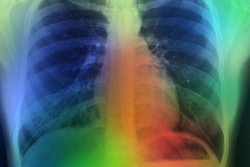
The team analyzed individual immune cells from human lung tumor samples taken from 68 people before they were treated with PD-1 inhibitors. They mapped the cells’ genetic activity as well as the location of the cells in the tumors.
The researchers found organized hubs of immune cells, or immunity hubs, within some tumors. Tumors from people who responded well to PD-1 blockers tended to have a subtype of hub, called stem-immunity hubs, that consisted of specific types of immune cells and signaling molecules known to drive effective antitumor responses, according to a report on the Broad Institute’s website.
Nir Hacohen, co-senior author of the study, an institute member at Broad and director of the Center of Cancer Immunology at MGH, and Jonathan Chen, co-first author, a member of the Hacohen Lab and investigator in the department of pathology, have described their findings and how they are now translating them into potential diagnostics and therapeutics.
In 2021, Hacohen and Chen reported the discovery of immunity hubs in colorectal cancer; however, the patients in the study were not treated with immunotherapy.
“In this new study, we sought to answer whether immunity hubs are indeed predictive of response to standard of care immunotherapy. We studied non-small cell lung cancer (NSCLC), which is commonly treated with PD-1 blockade immunotherapy,” they said.
“We found that patients without immunity hubs in their tumors prior to PD-1 blockade therapy had poor outcomes relative to patients with hubs. Critically, we discovered the stem-immunity hub, a subtype of immunity hub that is strongly associated with favorable immunotherapy response,” added the two authors.
They explained that a high-resolution spatial approach allowed them to discover important cell–cell interactions that may regulate the formation and function of these hubs.
“We found that patients without immunity hubs in their tumors prior to PD-1 blockade therapy had poor outcomes relative to patients with hubs.
Critically, we discovered the stem-immunity hub, a subtype of immunity hub that is strongly associated with favorable immunotherapy response,” they said.
Hacohen and Chen say stem-immunity hubs were enriched for a type of T cell that is remarkable for its ability to divide and invigorate the antitumor immune response after PD-1 blockade.
“So the finding of these stem-immunity hubs represents a new way to think about how the immune response is organized in human cancer.”
The team hopes to use the presence of the immunity hub, particularly the stem-immunity hub subclass, as a biomarker to predict response to immunotherapy.
“The current standard biomarker for prediction of immunotherapy response is PD-L1 antibody staining, but it can be inaccurate and difficult to use. We are currently testing a simple two-marker tissue stain that reflects immunity and can be assessed by pathologists using a standard workflow,” the authors wrote.