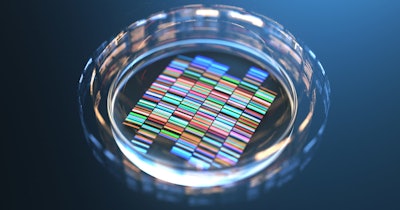
A next-generation sequencing (NGS) test provides high sensitivity in determining which pancreatic cysts are likely to become cancerous, according to a large multicenter study published on Thursday in Gastroenterology.
By sequencing 22 pancreatic cyst-associated genes, the PancreaSeq test, developed by researchers at the University of Pittsburgh Medical Center, accurately distinguished benign cysts from those that could become cancerous, according to the study.
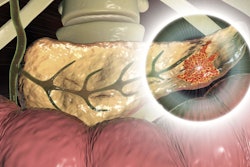
The test analyzes molecular markers in pancreatic cyst fluid collected from patients. Pancreatic cysts can be broadly categorized as either nonmucinous (benign) or mucinous, leading to the onset of pancreatic cancer.
In the study, PancreaSeq diagnosed mucinous cysts accurately in 90% of the cases, based on mutations in the oncology-related genes KRAS and GNAS. Furthermore, it did not identify any false positives, giving it 100% specificity.
“In comparison, other modalities and current pancreatic cyst guidelines, such as the AGA (American Gastroenterological Association) and IAP (InterAcademy Partnership)/Fukuoka guidelines, show inferior diagnostic performance,” wrote Dr. Alessandro Paniccia, a researcher at the University of Pittsburgh Medical Center and the first author of the study, and colleagues.
Their objective was to capture the population of patients with pancreatic cysts and confirm that PancreaSeq is useful in a clinical setting. They applied a prospective study design, scrutinizing molecular markers in pancreatic cyst fluid collected from patients and following outcomes.
Prospective PancreaSeq testing was performed between January 2018 and February 2020. The testing involved 1,933 pancreatic cyst fluid specimens obtained by endoscopic ultrasound/fine-needle aspiration which had been submitted to the scientists from 31 medical institutions.
Among the 1,933 specimens prospectively tested, 1,887 specimens from 1,832 patients were found satisfactory for PancreaSeq testing. Follow-up was available for 1,216 patients. Based on 251 patients with surgical pathology, MAPK/GNAS mutations had 90% sensitivity and 100% specificity for a mucinous cyst. The combination of MAPK/GNAS and other genes -- TP53/SMAD4/CTNNB1/mTOR alterations -- had 88% sensitivity and 98% specificity for advanced neoplasia, according to the researchers.
When they included another type of analysis -- evaluation of cells under the microscope for cancer-associated changes -- the test sensitivity improved to 93%. Specificity remained high at 95%.
Current PC guidelines for the most part have focused on detecting advanced neoplasia in intraductal papillary mucinous neoplasms (IPMNs). The investigators undertook a subanalysis of PancreaSeq testing combined with cytopathologic evaluation of 167 resected IPMNs. They found sensitivity and specificity of 88% and 96%, respectively.
Comparing the absolute criteria for surgical management from the AGA guidelines and the IAP/Fukuoka guidelines showed lower sensitivities of 72% and 86% and lower specificities of 66% and 36% compared to PancreaSeq and cytopathologic evaluation.
The researchers believe that the advantage of PancreaSeq testing is its high specificity for advanced neoplasia. In contrast, the AGA guidelines and the IAP/Fukuoka Guidelines exhibit low-to-moderate specificity but moderate-to-high sensitivity, they said, adding that the low-to-moderate specificity of both guidelines is not surprising since they rely on subjective and indirect features of advanced neoplasia, such as large -- greater than 3.0 cm -- pancreatic cyst size, main pancreatic duct dilatation, and the presence of a mural nodule on endoscopic ultrasound, the scientists wrote.
According to the researchers, the results of the study generally underscore the clinical utility of targeted NGS, given its high sensitivity and high specificity in diagnosing mucinous cysts and identifying advanced neoplasia within a mucinous cyst.