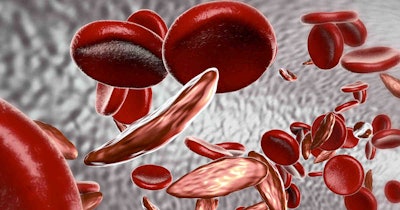
Researchers have created a preclinical proof-of-concept model for using mRNA to engineer bone marrow cells inside patients to treat blood disorders including sickle cell disease.
Writing in the journal Science, researchers at Children's Hospital of Philadelphia and the Perelman School of Medicine at the University of Pennsylvania described a way to modify hematopoietic stem cells (HSCs) in vivo through the delivery of mRNA. If shown to work in humans, the approach could address problems with current treatments for blood disorders.
Transplanting bone marrow from healthy donors can cure certain blood disorders but it carries the risk of graft-versus-host disease (GvHD), relies on donors, and requires patients to receive chemotherapy or radiation. The GvHD risk is mitigated by using a patient’s own cells, which are harvested, engineered, and transplanted back in, but that approach still requires conditioning with chemotherapy or radiation.
Performing the editing in vivo could eliminate the need for donor cells and the use of potentially toxic conditioning regimens. Messenger RNA, the nucleic acid used in leading COVID-19 vaccines, could enable the in vivo editing.
One problem is that, unlike COVID-19 vaccines, a treatment for sickle cell would need to target specific cells. To facilitate that targeting, the authors of the Science paper added anti-CD117 antibodies to the lipid nanoparticles (LNPs) they created to deliver mRNA. Because CD117 is found on the surface of HSCs, the antibodies could direct the LNPs to the cells and enable targeted gene editing.
The delivery of the editing system resulted in the near-complete correction of hematopoietic sickle cells. A preclinical test linked the approach to a 91.7% increase in functional hemoglobin and a significant fall in the number of sickled cells.
Building on their work, the scientists used the CD117-directed LNPs to make a drug candidate that could deplete bone marrow without the use of chemotherapy or radiotherapy. The conditioning LNPs deliver the mRNA for PUMA, a protein that promotes cell death. In animal models, the candidate depleted HSCs and enabled engraftment rates consistent with those seen in patients cured by cell transplants.