A CRISPR system that uses Cas13d to make reversible changes to the expression of multiple genes could overcome limitations that are holding back CAR-T cell therapies, a paper published in Cell suggests.
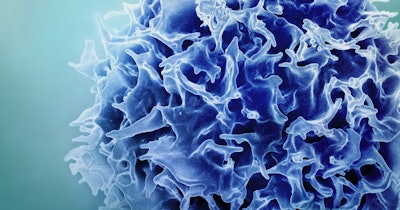
CAR-T therapies can cause complete responses in people with certain blood cancers. However, attempts to bring those benefits to more patients have been stymied by primary or acquired resistance and a lack of efficacy in solid tumors. Researchers have identified phenomena such as T-cell exhaustion as a cause of these problems.
Genetic engineering could create cells that are less prone to exhaustion, enabling them to keep attacking hard-to-penetrate solid tumors for longer periods, but editing the cells can create other problems. CRISPR-Cas9, which cuts DNA, can cause potentially genotoxic side effects.
A team at Stanford University identified Cas13d as a potential solution to the gene-editing problem. The nuclease complexes with a CRISPR-associated RNA, rather than cutting DNA like Cas9. Because Cas13d acts on RNA not DNA, it could trigger the desired changes to gene expression in T cells without making the permanent edits associated with safety concerns.
Cas13d has other potential benefits over its better-known counterpart. The nuclease is around two-thirds of the size of Cas9, making it well suited to T-cell manufacturing, and can more easily target multiple genes at once.
The Stanford researchers provided early validation of the approach by making up to 10 edits at the same time. Through the changes, the team created CAR-T cells that performed “10 times better, in terms of reducing the tumor growth and in terms of sustaining long term T cell proliferation,” Stanley Qi, Stanford associate professor of bioengineering and senior author of the Cell paper, said in a statement.
That 10-fold improvement was achieved by changing how the cells use sugar. Switching from a glycolysis process toward oxidative phosphorylation resulted in cells that persisted for longer in the tumor site. While the Cas13d cells were initially less effective, they kept going for longer and ultimately had a more powerful effect on tumors.
The Cas13d platform, which the researchers call MEGA, also enables the creation of CAR-T cells that can be controlled by drug compounds. By varying the dose of trimethoprim, an approved antibiotic, the team tuned gene expression. The approach, forms of which are being advanced by multiple groups, may make CAR-T therapies more controllable, as conventional medicines are, and thereby improve safety.
Immunogenicity is a potential barrier to clinical use, but the researchers have seen enough promise in the platform to outline plans for further work. Assessments of the impact of the platform on the efficacy of other CAR and T-cell receptor cells are among the studies proposed by the researchers.