Dear LabPulse Member,
I'm writing to you from the Bay Area of California, where we are under orders to stay at home aside from essential activities, such as grocery shopping. Our staff members are all working remotely, regularly watching press briefings, and staying on top of the large volume of news on the novel coronavirus outbreak for our readers.
Other states have followed suit with stay-at-home orders, and it's unclear how long this will go on. Layoffs and furloughs are mounting, while many people have been separated from their loved ones, particularly the elderly and immunocompromised.
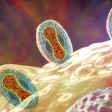
In its March 23 situation report, the World Health Organization (WHO) reported more than 332,000 confirmed COVID-19 cases globally, including over 171,000 in Europe. Worldwide, there have been more than 14,500 deaths, including over 8,700 in Europe.
In its latest situation report, the WHO once again stressed how critical diagnostic testing is for tracking the SARS-CoV-2 virus and noted that it has updated its laboratory testing strategy document.
Diagnostic tests are still reportedly in short supply, even though the U.S. Food and Drug Administration (FDA) has loosened restrictions on the performance of novel coronavirus testing to allow laboratory-developed tests to be conducted without an emergency use authorization (EUA).
The agency has also quickly granted a number of EUAs to vendors, including one to Cepheid for a new point-of-care (POC) test. The test has a number of advantages over other products, including the delivery of results in 45 minutes -- much faster than other tests approved so far, reported Bruce Carlson, publisher of market research firm Kalorama Information. No operator training is required to perform the test and determine a result, so it can be used in doctors' offices and retail clinics.
How might the overall picture look if the U.S. Centers for Disease Control and Prevention had not initially insisted on a centralized approach around its own novel coronavirus test, which turned out to be flawed when delivered to labs? The volume of testing we now see in March may have been available in February, Carlson said.
But even after the FDA issued guidance in late February allowing laboratory-developed tests to be used, these assays are still somewhat manual, low in volume, and require expertise at advanced medical center labs, Carlson told LabPulse.com. And shortages of personal protective equipment and other resources present barriers to the expansion of testing beyond the availability of testing equipment itself.
There are also financial uncertainties around lab-developed tests that need to be ironed out. The American Clinical Laboratory Association (ACLA) has asked the U.S. Congress for a $5 billion emergency fund to cover novel coronavirus testing, which the government has pledged will be provided for free to the public. Coverage of lab-developed tests without an EUA was not included in the Families First Coronavirus Response Act just passed by Congress, but the hope is that it will make the cut in other emergency legislative packages.
Some positive news related to COVID-19 recently emerged in the Archives of Pathology & Laboratory Medicine. A review of published reports in China concluded that pregnant women infected with SARS-CoV-2 did not have a higher rate of maternal deaths. We surely could use more good news like this amid the pandemic.
In other clinical news, a team of researchers identified 39 genes associated with group A Streptococcus, which can cause deadly female genital tract infections.
Finally, the pandemic has drawn more attention to digital pathology and artificial intelligence (AI) applications. In a new report, contributing writer and Kalorama analyst Shara Rosen reviews the promise of AI in clinical diagnostics -- as well as the controversies.