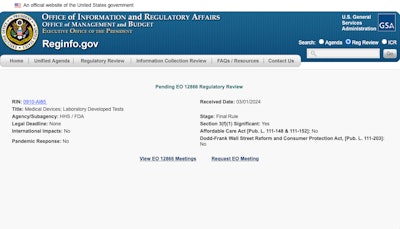
New directions in clinical laboratory-developed test (LDT) regulation appeared closer to decisions with the March 1 Office of Management and Budget (OMB) acceptance of the LDT final rule, pending regulatory review. Lab industry stakeholders took to LinkedIn this week to voice their opinions.
"It's a shame Congress didn't pass the VALID Act," wrote Dr. Scott Gottleib, a former U.S. Food and Drug Administration (FDA) commissioner who has joined the ranks of a venture capital firm, is an elected member of the National Academy of Medicine, and also serves on Pfizer's board of directors. "It [VALID Act] was a much more efficient vehicle for regulating this field; giving FDA more tools to implement a risk-based framework. Once the rule is implemented, it will be hard to get a second chance at the VALID Act."
VALID Act not impossible
Others, however, responded not to count out the VALID Act in 2024. Dr. Bruce Quinn, a consultant in the clinical laboratory industry, said VALID Act's odds are low but "above impossible."
In other efforts to get more voices heard over reforming LDT regulation, the New England Journal of Medicine (NEJM) featured a mixed bag of letters on February 1. Several readers took issue with the pro-FDA stance of an NEJM Perspective article by Drs. Udit Singhal and Todd Morgan, both from the University of Michigan, Ann Arbor, and Aaron Kesselheim of Brigham and Women's Hospital in Boston, that was published late last year.
While Singhal and colleagues raised doubt (as others also have) about weaknesses of the Clinical Laboratory Improvement Amendments (CLIA) system under the Centers for Medicare and Medicaid Services (CMS) and pointed fingers at commercial laboratory tests, others emphasized certain types of lab tests that will require very careful consideration should the controversial LDT rule come to pass.
ASTs, newborn screening, rare disease testing
Dr. Virginia Pierce of the University of Michigan Medical School defended antimicrobial susceptibility tests (ASTs), for which there is no regulatory pathway to seek FDA clearance. Chief among these are ASTs performed by laboratories for off-label pathogens.
Dr. Octavia Peck Palmer of the Association for Diagnostics and Laboratory Medicine (ADLM) brought up another popular LDT type, newborn screening tests.
Another letter highlighted LDTs' role in rare disease testing.
Drs. Singhal, Morgan, and Kesselheim responded with a letter of their own, saying that none of the areas of wide agreement should prevent policymakers from enhancing regulation regarding LDTs, particularly given the growing number of genetic tests being offered with unclear clinical validity at extremely high prices.
In addition, Singhal and colleagues held to their view that the FDA has the expertise to assess product performance, safety, effectiveness, and data appraisal in relation to the expanding volume of LDTs and the instruments used in their design. They also wrote that they were confident that LDTs would continue to be available should federal oversight change.
Proficiency testing gaps
Meanwhile, Archives of Pathology and Laboratory Medicine's February edition took a critical look at an important laboratory quality step, proficiency testing (PT). The article focused on next-generation sequencing (NGS) assays, a class of LDTs in practice in higher volume in recent years. Drs. Shuko Harada and Alexander Mackinnon, both of the University of Alabama, Birmingham, pointed out that College of American Pathologists (CAP) PT programs directly address and satisfy quality concerns of the FDA. They suggested the FDA endorse and promote existing CAP PT programs to monitor and ensure the quality and accuracy of LDTs.
However, Harada and Mackinnon also acknowledged that alternative PT is necessary to handle the "evolving landscape of laboratory testing" because laboratories frequently encounter situations where they must analyze new or emerging substances, employ customized testing methods, or cater to specific patient groups not covered by existing PT programs. They noted advanced forms of NGS testing, such as cell-free DNA analysis, saying, "There is a growing need to establish complementary or alternative PT assessment programs when an existing CAP PT is either not available or unsuitable for some reason."
New survey
Hospitals and health systems develop and use LDTs, as do academic medical centers and private commercial laboratories.
A new survey released March 5 reinforced that the proposed LDT rule, if enacted, will hurt clinical labs that perform LDTs. ARUP Laboratories said in a news release that the survey is the "largest exploration of the impact of the proposed rule on clinical laboratories to date." Most respondents identified themselves as lab managers, lab supervisors, lab directors, lab employees, medical directors, pathologists, physicians, clinicians, or PhD scientists. Full details were published at medRxiv.
Of 503 respondents, only 41 (8.2%) support the FDA's proposed rule, against the backdrop of nearly 85% feeling threatened, with just 3% believing they have the financial resources to pay FDA user fees, which can be as high as $483,000 for "high-risk" premarket authorization submissions, ARUP said. Additionally, nearly 61% of participants said they would likely remove tests from their laboratory menus if the proposed rule were to be enacted. One-third of respondents were not sure what they would do.
"Only a minority of respondents reported that they would likely either submit all of their LDTs, or more than half of their LDTs, for review if the FDA adopts the proposed rule," the full details stated.
The American Hospital Association has asked that the FDA continue to apply its enforcement discretion to hospital and health system LDTs and defer regulation of these laboratory tests mainly to CMS and strict CLIA oversight, CAP accreditation, and state law.