A pathology study of postmortem tissue with high-field magnetic resonance imaging (MRI) suggests that the nature of traumatic brain injury (TBI) is vascular, rather than being related to nerve damage, per conventional wisdom. The findings, published on October 14 in the journal Brain, open the door to new treatment strategies for concussion.
The prospective Traumatic Head Injury Neuroimaging Classification (THINC) study was funded by the U.S. Department of Defense and the National Institute of Neurological Disorders and Stroke (NINDS).
"Nerve damage following traumatic brain injuries has been a majority point of view, and therapy as well as drug development has been targeted towards that," co-author Partha Mitra, PhD, a professor at the Cold Spring Harbor Laboratory, said in a statement. "The idea is that if the mechanism is actually different, therapeutic intervention may also be different."
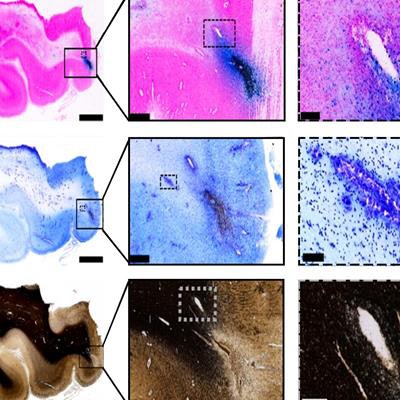
The researchers analyzed MRI studies of 439 subjects who had an acute brain injury. They assessed different types of injuries and how they matched with outcomes. For the study, postmortem brain tissue was sectioned and studied with 3- and 7-tesla MRI, including 3D reconstruction of histological sections. The researchers evaluated traumatic microbleeds (TMBs), which are small injuries that appear as areas of hypointensity on MRI, but often not on computed tomography (CT), and are associated with disability.
A new understanding
During the THINC study, a middle-aged man who had been in a bicycle accident died due to sepsis, and his family donated his brain for research. Digital pathological examination of brain tissue was performed at micron resolution and correlated with MRI, which the authors suggested provided a more accurate picture of the injury.
"This was an unusual opportunity because we had very good imaging right after the injury, at follow-up, and now could look at the acute findings on the corresponding pathology," NINDS scientist and senior author Lawrence Latour, PhD, explained in an email to LabPulse.com. "This is what changed our impression."
The researchers expected to find microbleeds primarily in the tissue, but they actually found little evidence of axonal damage, Latour said. Traditionally, traumatic microbleeds have been described as traumatic axonal injury or diffuse axonal injury. But that may be a misnomer that grew out of an association found between these small "bleeds" seen on MRI and axonal damage seen postmortem in more severe patients.
"We could easily see the large vessels on MRI, but there was a much broader network of vascular injury," Latour said. "Vascular injury after TBI is well known in animal models, but most of the field studying mild TBI/concussion in humans are focused on injury to the tissue."
In fact, damage to tissue may occur, but separately and discrete from the vascular injury.
 Tissue imaging confirms blood vessel damage in traumatic brain injury patients. Image courtesy of Mitra Lab/Cold Spring Harbor Laboratory.
Tissue imaging confirms blood vessel damage in traumatic brain injury patients. Image courtesy of Mitra Lab/Cold Spring Harbor Laboratory.The MRI studies also indicate that microbleeds are associated with ischemic damage, similar to what is seen with stroke, Latour said.
"This leads us to think that primary injury to the vessels occurs reasonably frequently in fairly minor head injury, and seems to result in greater residual disability," he said. "The hope is more attention is paid to therapies addressing the vessel injury, the ischemic/inflammatory damage right after, and long-term consequences related to inflammatory cells in the perivascular space."
Traumatic microbleeds are common
It's estimated that more than 2.5 million people are treated for traumatic brain injuries per year in the U.S. and 3 million people are living with disabilities as a result. The THINC study evaluated patients seen at trauma centers in Washington, DC, after a head injury requiring evaluation with CT. An MRI was done within 48 hours of the injury.
Traumatic microbleeds were common -- detected in 31% of cases overall -- and predictive of a worse outcome. They were reported in 58% of those with severe injuries, 47% with moderate injuries, and 27% with mild injuries. Patients with TMBs were twice as likely to exhibit disability 30 or 90 days after the injury, the researchers noted.
"TMBs are a common finding on MR images of patients following TBI," they wrote. "The field currently associates TMBs to both severe injury and clinical outcomes. However, our data suggest that TMBs are not exclusive to moderate or severe TBI."
Traumatic microbleeds may indicate who will benefit from treatments that minimize ischemic damage or improve microvascular cerebral blood flow, the researchers concluded.
"For example, pharmacological agents suggested by other TBI investigators to act on the microvasculature to increase cerebral perfusion include sildenafil and beta-blockers such as propranolol," they wrote. "In contrast, minocycline has the potential to reduce acute ischemic injury through its effects on inflammation, [the blood-brain barrier], and edema."