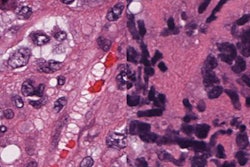
Stanford University researchers outlined a digital cytometry computational method that is useful for characterizing individual cells in intact tumor tissue samples. The technique could possibly predict response to cancer immunotherapy, according to a May 6 report in Nature Biotechnology.
The Stanford researchers describe their technique -- called CIBERSORTx -- as a machine-learning method that infers cell-type-specific gene expression profiles without the need for physical isolation of cells. The tool, which is an extension of their previously released CIBERSORT, incorporates information from reference datasets generated with single-cell sequencing.
With the computational method, it's possible to determine a pattern of RNA expression, or "barcode," to get detailed descriptions of particular kinds of cells. A barcode for immune cells infiltrating a tumor would differ from one for immune cells circulating in the blood, the authors explained.
"We anticipate that digital cytometry will augment single-cell profiling efforts, enabling cost-effective, high-throughput tissue characterization without the need for antibodies, disaggregation or viable cells," first author Aaron Newman, PhD, an assistant professor of biomedical data science at Stanford, and colleagues wrote in Nature Biotechnology.
CIBERSORTx is freely available to academic researchers via a dedicated website hosted by Stanford University.
Challenges of single-cell sequencing
The Stanford researchers developed the computational method in response to challenges associated with single-cell RNA sequencing.
With traditional immunophenotyping approaches such as flow cytometry and immunohistochemistry, the number of cell types that can be interrogated at the same time is limited. Single-cell sequencing makes it possible to profile thousands of individual cells from a single-cell suspension, but this is hard to achieve in practice due to the high cost and technical limitations, the authors noted.
"Despite the power of this technology, analyses of large sample cohorts are not yet practical, and most fixed clinical specimens ... cannot be dissociated into intact single-cell suspensions," Newman et al wrote. "Furthermore, the impact of tissue disaggregation on cell type representation is poorly understood."
In contrast with single-cell sequencing, CIBERSORTx may be used on tumor tissue samples that have been prepared in formalin and stored in paraffin, the authors wrote. The tool developed at Stanford "was designed to enable large-scale tissue characterization using cell signatures derived from diverse sources, including single-cell reference profiles."
"By leveraging cell type expression signatures from single-cell experiments or sorted cell subsets, CIBERSORTx can provide detailed portraits of tissue composition without physical dissociation, antibodies or living material," they wrote.
Connecting the dots in pharmaceutical response
The Nature Biotechnology article describes the use of CIBERSORTx in a range of tumor types, including non-small cell lung cancer, head and neck squamous cell carcinoma, follicular lymphomas, and melanomas.
"Oncogenic BRAF mutations occur in over half of melanomas and can be inhibited by approved targeted therapies, whereas NRAS mutations occur in approximately half of non-BRAF mutant melanoma tumors but lack such therapies," the researchers wrote. "Understanding how key mutations influence cellular states could potentially lead to new treatment strategies."
Potential applications of the method include predicting the response to treatment with checkpoint inhibitor immunotherapies targeted at programmed cell death 1 (PD-1) and cytotoxic T-lymphocyte antigen 4 (CTLA-4) proteins.
Some research has suggested that the presence of CD8 tumor-infiltrating T lymphocytes with high expression of PDCD1 (which encodes PD-1) and also CTLA-4 correlates with response in melanoma patients on PD-1 inhibitors.
A meta-analysis of three publicly available datasets by Newman et al using CIBERSORTx showed a significant association between high levels of CD8 T cells positive for PDCD1 and CTLA-4 and lower mortality rates. The association with response and survival was more robust than for key marker genes and other cell types, they noted.
"Given the rapid pace of data generation coupled with emerging techniques to combine [single-cell RNA-sequencing] datasets, methods to broadly apply single-cell reference maps will become increasingly important, especially in settings where tissue is limited, fixed or challenging to disaggregate into intact single cells," the authors concluded.
Methods for improving the selection of cancer immunotherapies are in high demand. In the past decade, checkpoint inhibitors have revolutionized the treatment of cancer and brought in billions for big pharma -- melanoma was the first major testing ground -- but response rates are still relatively low for many tumor types. The level of expression of programmed cell death ligand 1 (PD-L1) has been the most commonly used biomarker, but it is not accurate enough as a predictive test for use in directing drug treatment.
A study by researchers at Oregon Health and Science University (OHSU) published May 3 in JAMA Network Open found that in the U.S. in 2018, 43.63% of cancer patients were eligible for treatment with checkpoint inhibitors, but overall the percentage of responders was only 12.46%.
"The estimated percentages of patients who are eligible for and who respond to checkpoint inhibitor drugs are higher than reported estimates for drugs approved for genome-driven oncology but remain modest," Alyson Haslam, PhD, and Dr. Vinay Prasad from OHSU concluded.
"Future research should explore biomarkers to maximize the benefit of immunotherapy among patients receiving it," they wrote.