More microscopic studies of respiratory tract samples are needed in some patients with pneumonia to reduce the risk of treating drug-resistant infections, according to new guidance published on October 1 by the American Thoracic Society (ATS) and the Infectious Diseases Society of America (IDSA).
The new recommendations apply to the diagnosis and treatment of community-acquired pneumonia, from the time of signs and symptoms through treatment with antibiotics and follow-up chest imaging. They were published by a multidisciplinary team, including Dr. Joshua Metlay, PhD, chief of internal medicine at Massachusetts General Hospital (American Journal of Respiratory and Critical Care Medicine, October 1, 2019, Vol. 200:7, pp. e45-e65).
The guidance represents the first update from the ATS and IDSA on the topic since 2007. In a statement, the organizations said that an important difference this time around is their recommendation for more microscopic studies of respiratory tract samples in some subgroups of patients to avoid the prescription of therapies for conditions caused by drug-resistant bacteria.
| Community-acquired pneumonia guidance: Examples of changes | ||
| Test | 2007 | 2019 |
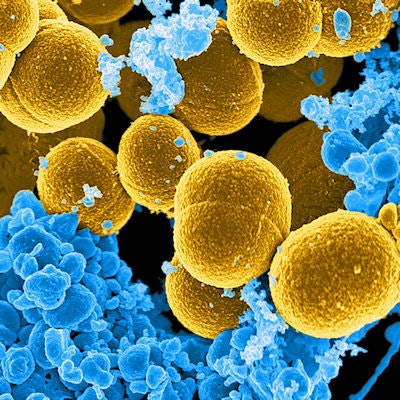
| Sputum culture | Primarily recommended in patients with severe disease | Now recommended in patients with severe disease as well as inpatients empirically treated for methicillin-resistant Staphylococcus aureus (MRSA) or Pseudomonas aeruginosa |
| Blood culture | Primarily recommended in patients with severe disease | Now recommended in patients with severe disease as well as all inpatients treated for MRSA or P. aeruginosa |
Since the last version was published in 2007, the process for guideline development has changed and new clinical data have become available. The old version was formatted in the style of graded recommendations, whereas the new release is presented as a series of questions and answers based on available evidence and a consideration of various options.
Antibiotics are used to treat the following bacterial pathogens, the authors noted:
- Streptococcus pneumoniae
- Haemophilus influenzae
- Mycoplasma pneumoniae
- S. aureus
- Legionella species
- Chlamydia pneumoniae
- Moraxella catarrhalis
"The microbial etiology of [community-acquired pneumonia] is changing, particularly with the widespread introduction of the pneumococcal conjugate vaccine, and there is increased recognition of the role of viral pathogens," the authors acknowledged.
"As bacterial pathogens often coexist with viruses and there is no current diagnostic test accurate enough or fast enough to determine that [community-acquired pneumonia] is due solely to a virus at the time of presentation ... our recommendations are to initially treat empirically for possible bacterial infection or coinfection," they wrote.
Separate recommendations are needed for multidrug-resistant pathogens for patients at higher risk, they added.