Scientists have fabricated an assay that can efficiently detect minute concentrations of alpha synuclein seeds in blood serum.
Their research, published Tuesday in Nature Medicine, has the potential to enable a quicker diagnosis of specific neurodegenerative disorders than is currently possible.
Synucleinopathies are a group of neurodegenerative diseases caused by the abnormal accumulation of alpha synuclein (α-synuclein), a protein normally found in the brain and neurons. Incorrect folding of α-synuclein leads to the formation of “seeds,” which attract more α-synuclein proteins to form larger clumps. Although α-synuclein seeds have been found in the blood of patients with synucleinopathies, its potential as a biomarker was unknown.
The researchers sought an assay that could efficiently detect α-synuclein seeds in blood serum. Using their assay, named immunoprecipitation-based real-time quaking-induced conversion (IP/RT-QuIC), the α-synuclein seeds are first isolated from the patient’s serum through immunoprecipitation — protein separation using an antibody binding only to the target protein. This is followed by rapid amplification induced by vigorous shaking. This highly sensitive method can detect serum α-synuclein seed concentrations as small as 1000pg/mL, an advantage over most existing diagnostic methods, which require cerebrospinal fluid for synuclein detection.
The team demonstrated that IP/RT-QuIC could efficiently detect α-synuclein seeds in patients with neurodegenerative diseases, and could distinguish these patients from a disease-free control group. They then studied the structural properties of the amplified seeds using transmission electron microscopy.
They observed that the synuclein seed structure varied with the type of synucleinopathy. The IP/RT-QuIC assay could also discriminate between the morphology of the fibrils, or threadlike structures, within the α-synuclein seeds in the serum of patients with Parkinson’s disease, dementia with Lewy bodies, and multiple system atrophy. Parkinson’s disease and dementia with Lewy bodies seeds both showed paired filaments, whereas multiple system atrophy seeds had two distinct structures, twisted and straight filaments, confirming that IP/RT-QuIC coupled with transmission electron microscopy could differentiate between synucleinopathies based on disease-specific seed structure.
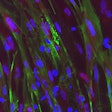
The researchers used transduction — the process by which foreign DNA is introduced into a cell by a viral vector — to introduce amplified seeds into an HEK293T cell line stably expressing human α-synuclein with p.A53T mutation, which in mice leads to motor deficits, paralysis, and death. The α-synuclein was fused with a green fluorescent protein tag to facilitate its visualization by fluorescence microscopy in vitro. The researchers also injected the seeds into mouse brains in vivo.
In both cases the seeds retained their aggregate forming capacity and disease-specific seed structure. These aggregates displayed different morphologies depending on the disease type. The researchers concluded that specific synucleinopathies can be diagnosed by IP/RT-QuIC from the structural differences of the α-synuclein seeds and aggregates, potentially providing quick, efficient patient diagnoses.
“At present, a neurologist's consultation is necessary to diagnose synucleinopathies,” co-author Dr. Nobutaka Hattori, of Juntendo University Faculty of Medicine, said in a statement. “However, using IP/RTQuIC, a general internist can make the diagnosis. Therefore, more patients with synucleinopathies may be diagnosed with precision and could receive appropriate treatment at an earlier stage.”
For that to happen, the technology would need to be further developed as part of a clinical test and approved by regulatory authorities.