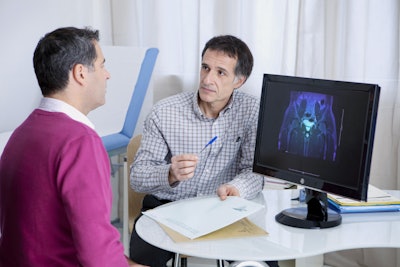
Higher screening rates for prostate-specific antigen (PSA) are associated with lower subsequent rates of metastatic prostate cancer, according to research published Monday in JAMA Oncology.
The research results may boost PSA testing among men, suggesting that screening is worthwhile to lessen their risk of prostate cancer.
Since 2008, PSA screening rates have decreased in the U.S., while the incidence of metastatic prostate cancer has increased. Although PSA testing results can help care providers and patients work together to select appropriate prostate cancer treatments and care plans based on clinical evidence, there has been no direct epidemiologic evidence of a correlation between population PSA screening rates and subsequent metastatic prostate cancer rates.
Investigators from the University of California at San Diego and colleagues elsewhere undertook a retrospective cohort study of patients at Veterans Health Administration (VHA) facilities to determine whether facility-level variations in PSA screening rates could be associated with subsequent facility-level metastatic prostate cancer incidence.
They used data for all men aged 40 years or older at 128 VHA facilities from January 1, 2005, to December 31, 2019. The cohort included 4,678,412 men in 2005 and 5,371,701 men in 2019.
The study found that when PSA screening rates decreased from 47.2% in 2005 to 37.0% in 2019, metastatic prostate cancer incidence increased from 5.2 per 100,000 men in 2005 to 7.9 per 100,000 men in 2019.
From 2005 to 2019, PSA screening rates decreased in the national VHA system. Higher facility-level PSA screening rates were associated with lower metastatic prostate cancer incidence five years later, and higher long-term nonscreening rates were associated with higher metastatic prostate cancer incidence five years later, the researchers found.
"The findings suggest that variation in prostate cancer screening rates is associated with subsequent metastatic prostate cancer incidence; these data may inform shared decision-making about the potential benefits of prostate-specific antigen screening," wrote the study’s lead author Dr. Alex Bryant of the Department of Radiation Oncology, Veterans Affairs Ann Arbor Health System in Michigan.
In 2008, when randomized clinical trials did not produce a consensus regarding the clinical benefit of PSA screening, the U.S. Preventive Services Task Force (USPSTF) recommended against PSA screening for men older than 75 years of age. This recommendation was followed by guidelines in 2012 recommending against PSA screening among men of any age.
After the 2012 guidelines, several studies demonstrated that there was a significant decrease in nonmetastatic prostate cancer incidence associated with a decrease in PSA screening rates. However, at the same time, the decrease in nonmetastatic prostate cancer incidence was accompanied by a significant increase in metastatic prostate cancer incidence from about 2013 onward.
Negative mortality results from the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial that were published in 2009 may also have contributed to decreasing screening rates, the researchers conjectured.
The investigators indicated that their study results may implicate PSA screening behaviors in subsequent metastatic prostate cancer incidence.
This would be consistent with findings from the European Randomized study of Screening for Prostate Cancer (ERSPC) trial, which demonstrated decreased metastatic prostate cancer incidence in the trial’s PSA screening arm compared with the usual-care arm.
The investigators’ finding of an association between lower facility-level PSA screening rates and higher subsequent metastatic prostate cancer incidence provides epidemiological support for the ERSPC trial results, they stated.
Policies that increase PSA screening among eligible veterans might lead to decreases in future incidences of metastatic prostate cancer. The cohort study findings also highlighted a potential need for policies that reduce interfacility variation in PSA screening behaviors, particularly among older age groups.