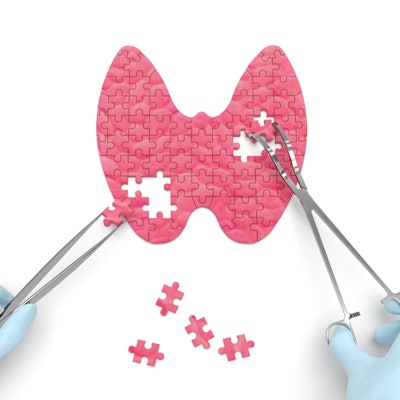
Thyroid function screening should not be done in the primary care setting for nonpregnant adults without symptoms or risk factors, according to a new Canadian guideline released on November 18. Such liberal screening is currently common in the U.S. and Canada.
The guideline was developed by the Canadian Task Force on Preventive Health Care, which published its recommendations in the Canadian Medical Association Journal (November 18, 2019, Vol. 191:46, pp. E1274-E1280). The recommendations are based on a review of the evidence, which is very limited for thyroid function screening. They do not apply to patients with previously diagnosed thyroid disease or thyroid surgery, among other specified populations.
Function is assessed by measuring levels of thyroid-stimulating hormone (TSH). Measuring TSH is appropriate for those with certain signs and symptoms, including fatigue, weight gain, and menstrual irregularities, and for those at risk of thyroid dysfunction due to pituitary disease and other secondary causes, explained Dr. Richard Birtwhistle, director of the Centre for Studies in Primary Care at Queen's University in Kingston, Ontario, and colleagues.
The task force did not evaluate total cost as part of the review, but the authors noted that it would include the TSH test, which costs $5 to $14, as well as other expenses such as those related to diagnostic tests, fees, and monitoring.
"In the judgment of the task force, given the lack of evidence of clinical effectiveness, financial costs of screening asymptomatic adults would represent an undesirable consequence for the [healthcare] system," Birtwhistle et al wrote.
Swimming against the TSH tide
The guideline represents a big change from the status quo. Currently, thyroid function screening is not part of formal programs in Canada, yet it is commonly ordered for asymptomatic people. The authors noted that 10% of Canadians older than 45 reportedly have been diagnosed with thyroid dysfunction -- 16% of women and 4% of men. Recommending against screening "would reduce unnecessary tests and burden on patients," they advised.
The Canadian Task Force on Preventive Health Care's stance is in line with some other sets of guidelines from Canada but differs from U.S. reviews (see table).
| Comparison of guidelines on TSH screening | |
| Canadian Task Force on Preventive Health Care | Routine thyroid function testing is not recommended in asymptomatic adults. Testing may be indicated when there are signs and symptoms in patients at risk for thyroid disease. |
| British Columbia Ministry of Health | Routine thyroid function testing is not recommended in asymptomatic adults. Testing may be indicated when there are signs and symptoms in patients at risk for thyroid disease. |
| Toward Optimized Practice (Alberta, Canada) | Do not test patients who are asymptomatic, seemingly healthy, and having a periodic exam. |
| U.S. Preventive Services Task Force | Current evidence is insufficient to assess benefits and harms of screening in asymptomatic adults. |
| American Thyroid Association and American Association of Clinical Endocrinologists | Screening for hypothyroidism should be considered in patients older than 60 years. |
Notes from across the border
In a commentary on the guideline published in the same issue of CMAJ (pp. E1260-E1261), endocrinology specialists Dr. Omar El Kawkgi and Dr. Juan Brito from the Mayo Clinic in Rochester, MN, noted that thyroid disease is rare in asymptomatic people who have one abnormal TSH test result.
"In a study following outpatients without thyroid disease over [five] years, 62% of TSH values normalized on subsequent testing without any intervention, which could be explained in part by variations in TSH secretion," Kawkgi and Brito wrote. "Furthermore, TSH values are also affected by drugs, autoimmune diseases and problems with interference in the analytical assay, which can lead to false positives that result in misclassification of people with no clinical evidence of thyroid dysfunction."
Finding asymptomatic thyroid dysfunction may lead to treatment with levothyroxine (Synthroid and other brands), which has not demonstrated a significant benefit in this population, the editorial authors wrote. In fact, in the U.S., the number of levothyroxine prescriptions rose from 97 million in 2007 to 120 million in 2014. More use of the drug means more chances for treatment complications and increased utilization of associated healthcare resources, they suggested.
"The recommendation against screening from the Canadian task force is the latest addition to recommendations for other clinical practices highlighting the potential harms of screening for asymptomatic people who may not always benefit from finding or treating conditions early," Kawkgi and Brito wrote.
This may help prevent the overdiagnosis of "otherwise healthy people," but on the other hand, the guideline was based on low-quality evidence, and more research is needed to guide practice in subgroups that may benefit, they concluded.
Money talks
Reimbursement may have a bigger effect on practice than guidelines. The American Thyroid Association and the American Association of Clinical Endocrinologists advise screening for people older than 60, which translates into an eligible population of 60 million people in the U.S., Kawkgi and Brito noted.
However, the U.S. Medicare program does not cover TSH testing/screening of asymptomatic enrollees and limits monitoring of stable disease to two tests per year, per a national coverage determination (NCD) policy. Dr. Clayton Wilburn, a spokesman for the College of American Pathologists (CAP), commented in an interview that Cigna and other major payors have followed Medicare's lead and implemented similar restrictions on coverage in recent years.
"As the individual providers are contacted by the compliance officers at the hospital systems in their local areas with concerns of noncoverage of their patients, that could also help change the tune overall," added Wilburn, who is medical director of clinical chemistry, immunology, and point-of-care testing at the University of Vermont Medical Center.